How BEC Clinical Content Supports QBPs
 Quality-based procedures (QBPs) are clusters of patient groups that have been identified by the Government of Ontario as offering an opportunity for care improvement and cost reduction. Patient-based funding in Ontario is now partially based on QBP performance.
Quality-based procedures (QBPs) are clusters of patient groups that have been identified by the Government of Ontario as offering an opportunity for care improvement and cost reduction. Patient-based funding in Ontario is now partially based on QBP performance.
The move toward a patient-centred, evidence-informed funding model requires significant changes in how care is documented and provided. QBPs require the collection and analysis of data that is captured during various stages of a patient journey. In the Emergency Department (ED), activities during this journey include: taking a patient history; performing a physical examination; reassessments as required; performing procedures; placing orders; reviewing results; and ultimately disposition of the patient. Documentation of this activity is becoming more important (you don’t do what you don’t document).
For many of the conditions now measured for QBP funding purposes, the scope of the episode of care begins in the ED. Patients presenting with hip fractures, congestive heart failure (CHF), chronic obstructive pulmonary disease (COPD), or stroke typically arrive in the ED. The care a patient receives in the ED therefore has a disproportionate effect on patient outcomes and patient-based funding.
Once a patient arrives in an ED, the care provided and decisions made by practitioners result in large variations in admission rates. For example, while ED admission rates across Ontario average 63% for CHF, hospitalization rates vary from 39 to 99 per 100,000 residents across regional health networks. These variations suggest that: (1) the use of evidence to make admission decisions is uneven; and (2) some hospitals are performing unnecessary diagnostic tests and treatments.
To take full advantage of patient-based funding, hospital administrators’ objectives should be to maximize quality of care for QBPs while optimizing the resources required to diagnose, treat, measure, and report.
Providing effective and integrated clinical decision support at the initial point of care encourages the adoption of best practices and allows practitioners to risk stratify many of these patients (e.g. for CHF, COPD, and stroke patients). Clinical decision support at the point of care also allows hospitals to optimize admission rates and reduce unnecessary tests.
Example 1: Optimizing Admission Rates
In an ideal scenario, every patient who needs further investigation, treatment, or observation would be admitted while avoiding any unnecessary usage of hospital resources. For many conditions, evidence-based guidelines exist to help ED practitioners determine if patients require further care. However, these guidelines are often complex and difficult to use at the point of care without the implementation of appropriate clinical decision support.
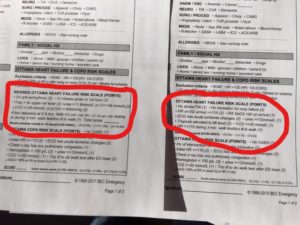
For CHF, the QBP Clinical Handbook recommends the use of the EHMRG tool to stratify patients according to risk. This helps reduce unnecessary admissions while reducing the odds of mistakenly discharging the wrong patient. Using BEC clinical content as part of your electronic or paper-based documentation allows emergency physicians to remember and effectively apply the EHMRG tool (or other alternative tools if you prefer) at the point of care, reducing unnecessary tests and admissions.
Other QBPs and various conditions also have clinical assessment tools that, if properly applied, optimize admission rates. For COPD, tools such as GOLD criteria and the Ottawa COPD rule help to correctly identify patients who need hospital admission – a QBP indicator. BEC content integrates these rules into the documentation process, allowing practitioners to apply them uniformly.
Example 2: Determining Stroke Types
According to the QBP Clinical Handbook, “stroke types should be specified for all admissions”. The handbook also acknowledges that “a large proportion of strokes are not specified as hemorrhagic or ischemic”. As well, the recognition of a stroke versus a mimic is often difficult to accomplish in the ED.
By incorporating best evidence research “Is this patient having a stroke” criteria and screening assessment tools such as the Canadian Neurological Scale and the NIHSS into physician workflow, BEC Clinical Content improves documentation of the neurological component of examinations and helps practitioners determine if and what type of stroke has occurred.
Example 3: How Procedure and Result Notes Improve Outcomes
Patient outcomes are best when physicians provide evidence-based care. While practitioners endeavor to provide the best care possible, the complexity and fluidity of medical evidence makes it difficult for physicians to stay current. By providing reminders at the point of care and during the documentation of treatments and results, health care providers are better able to accurately provide evidence-based care.
For example, there are patient preferences for care, indications and contraindications when performing non-invasive positive pressure ventilation (NPPV) for COPD patients. By using an NPPV procedure note that identifies these items, physicians can both practice better medicine and quickly document their actions.
Similarly, there are several observations that should be made when reviewing a CT scan for signs of stroke. By using a result note that includes these observations, physicians can quickly and accurately assess the likelihood of a stroke having occurred and the patient’s eligibility for thrombolytic therapy.
BEC procedure and result notes include the indications, contraindications, and observations required to improve patient outcomes for QBP reporting.
Conclusion
The advent of quality-based funding means that hospitals need to change how they deliver and document care. Dramatic improvements to patient outcomes measured for QBP purposes can be made by integrating clinical decision support at the point of initial care in the ED. By making correct decisions in the emergency department before admission or disposition, hospitals can improve their QBP performance and ranking.
 Previous Post
Previous Post Next Post
Next Post