What to do when you spend more time with your EHR than with your patients
The recent AJEM article 4000 Clicks: a productivity analysis of electronic medical records in a community hospital ED has gotten a fair bit of attention, and rightly so. The article points out several troubling facts for EDs that have adopted EHRs or that are considering doing so:
- 43% of physicians’ time spent on data entry
- 28% of time in direct patient contact
- 13% in discussions with colleagues
- 12% reviewing tests and records
While the amount of concern about time spent on data entry should be high, there are two clear follow-up questions:
- How does this compare to paper charting?
- What can we do about it?
We have answers for both.
1. How does this compare to paper charting?
Short answer: not well, but not too badly.
Longer answer: it’s hard to do a direct comparison, because other studies count differently. For example, this article in the Danish Medical Journal used semi-structured paper charts, and doctors in the ED spent 25% of time in direct patient contact vs. 31% of their time documenting.
What’s clear is this particular paper-based ED spends less time on documentation than this particular electronic-ED. It’s hard to know the extent to which this can be extrapolated to other hospitals, and it’s difficult to say how much the time difference is related to the paper-based charting being structured and the EHR using a slow method of data entry (we know structure reduces documentation time by 25-30%). There are also other factors at play, such as different workflow, regulatory requirements, physicians, presenting cases, etc.
2. How can you spend less time documenting – without compromising patient care?
It’s hard to draw firm conclusions about whether and how much an EHR slows documentation in the ED. We do, however, know how to reduce documentation time.
- Add structure and clinical content: structure, templates, and clinical content do more than reduce the frequency of errors. By pre-filling parts of the document, they can reduce documentation time by 30%. What’s important is that your ED has sufficient templates to cover most complaints and assessments. It takes over 200 complaint templates to cover 90% of presenting cases. Structure can reduce documentation time by 30 minutes over an 8 hour shift.
- Provide faster options for data entry: typing and dictation are slow (and can lead to mistakes). A faster option is using voice macros, where the physician dictates into a structured chart. The fastest (and least likely to cause mistakes) option is to use touch-screen evidence-based templates.
- Make sure workflow is patient-oriented instead of technology-oriented: documentation should occur where you want, not necessarily where there’s a bank of computers. ED physicians walk 10 km/6 miles per shift. No wonder they aren’t spending more time with patients!
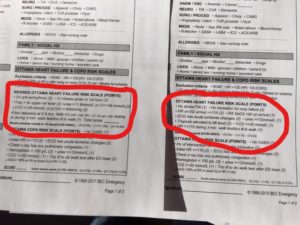
BEC Clinical Content and Clinical Decision Support Tools come with evidence-based assessments, differential diagnoses, and order sets to cover almost all cases in the ED. These templates can be added to most EHR systems to help prevent physicians from spending more time with a computer than with patients.

 Previous Post
Previous Post Next Post
Next Post